Head injury: types of traumatic brain injury
Basics
- primary brain injury may be focal (contusion/haematoma) or diffuse (diffuse axonal injury)
- diffuse axonal injury occurs as a result of mechanical shearing following deceleration, causing disruption and tearing of axons
- intra-cranial haematomas can be extradural, subdural or intracerebral, while contusions may occur adjacent to (coup) or contralateral (contre-coup) to the side of impact
- secondary brain injury occurs when cerebral oedema, ischaemia, infection, tonsillar or tentorial herniation exacerbates the original injury. The normal cerebral auto regulatory processes are disrupted following trauma rendering the brain more susceptible to blood flow changes and hypoxia
- the Cushings reflex (hypertension and bradycardia) often occurs late and is usually a pre terminal event
| Type of injury | Notes |
|---|---|
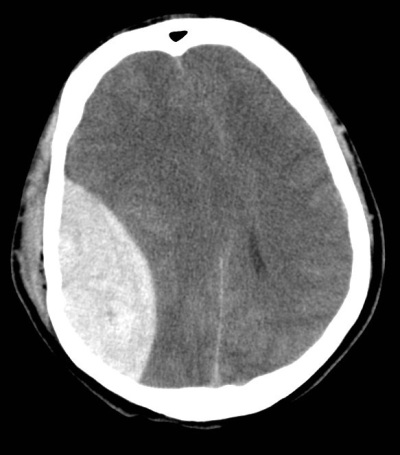
| Extradural (epidural) haematoma |
Bleeding into the space between the dura mater and the skull. Often results from acceleration-deceleration trauma or a blow to the side of the head. The majority of epidural haematomas occur in the temporal region where skull fractures cause a rupture of the middle meningeal artery.
Features
- features of raised intracranial pressure
- some patients may exhibit a lucid interval
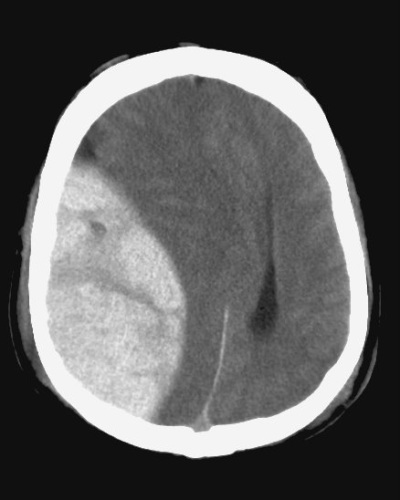
| | Subdural haematoma | Bleeding into the outermost meningeal layer. Most commonly occur around the frontal and parietal lobes.
Risk factors include old age, alcoholism and anticoagulation.
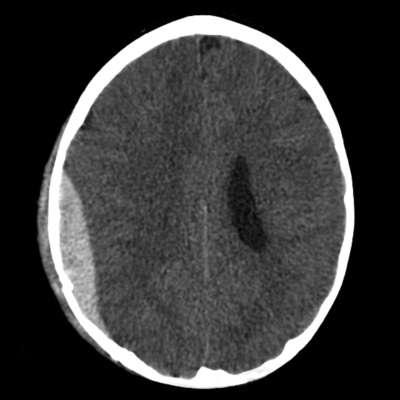
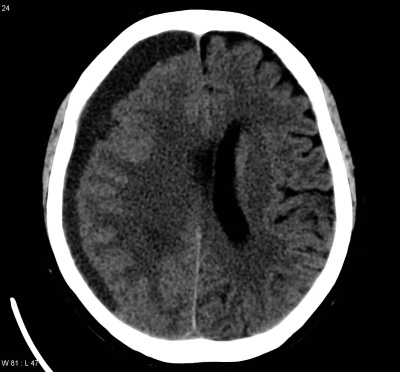
Slower onset of symptoms than a epidural haematoma. There may be fluctuating confusion/consciousness | | Subarachnoid haemorrhage | Classically causes a sudden occipital headache. Usually occurs spontaneously in the context of a ruptured cerebral aneurysm but may be seen in association with other injuries when a patient has sustained a traumatic brain injury | | Intracerebral haematoma | An intracerebral (or intraparenchymal) haemorrhage is a collection of blood within the substance of the brain.
Causes / risk factors include: hypertension, vascular lesion (e.g. aneurysm or arteriovenous malformation), cerebral amyloid angiopathy, trauma, brain tumour or infarct (particularly in stroke patients undergoing thrombolysis).
Patients will present similarly to an ischaemic stroke (which is why it is crucial to obtain a CT in head in all stroke patients prior to thrombolysis) or with a decrease in consciousness.
CT imaging will show a hyperdensity (bright lesion) within the substance of the brain.
Treatment is often conservative under the care of stroke physicians, but large clots in patients with impaired consciousness may warrant surgical evacuation. |
Image gallery
Extradural (epidural) haematoma:
Subdural haematoma:
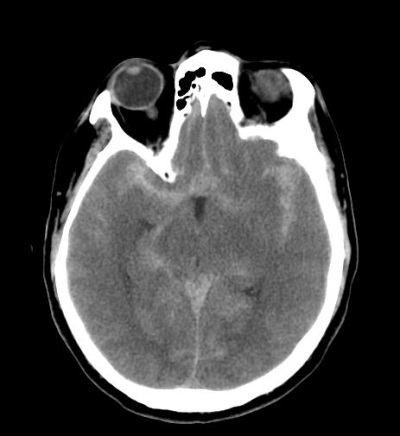
Subarachnoid haemorrhage: