pulmonary embolism - Investigations
We know from experience that few patients (around 10%) present with the textbook triad of pleuritic chest pain, dyspnoea and haemoptysis. Pulmonary embolism can be difficult to diagnose as it can present with virtually any cardiorespiratory symptom/sign depending on its location and size.
So which features make pulmonary embolism more likely?
The PIOPED study1 in 2007 looked at the frequency of different symptoms and signs in patients who were diagnosed with pulmonary embolism.
The relative frequency of common clinical signs is shown below:
- Tachypnea (respiratory rate >20/min) - 96%
- Crackles - 58%
- Tachycardia (heart rate >100/min) - 44%
- Fever (temperature >37.8°C) - 43%
It is interesting to note that the Well's criteria for diagnosing a PE use tachycardia rather than tachypnoea.
All patients with symptoms or signs suggestive of a PE should have a history taken, examination performed and a chest x-ray to exclude other pathology.
Pulmonary embolism rule-out criteria (PERC)
NICE updated their guidelines on the investigation and management of venous thromboembolism (VTE) in 2020. One of the key changes was the use of the pulmonary embolism rule-out criteria (the PERC rule)
- a copy of criteria can be found in the image below
- all the criteria must be absent to have negative PERC result, i.e. rule-out PE
- this should be done when you think there is a low pre-test probability of PE, but want more reassurance that it isn't the diagnosis
- this low probability is defined as < 15%, although it is clearly difficult to quantify such judgements
- a negative PERC reduces the probability of PE to < 2%
- if your suspicion of PE is greater than this then you should move straight to the 2-level PE Wells score, without doing a PERC
2-level PE Wells score
If a PE is suspected a 2-level PE Wells score should be performed:
| Clinical feature | Points|
Clinical signs and symptoms of DVT (minimum of leg swelling and pain with palpation of the deep veins)
3
An alternative diagnosis is less likely than PE
3
Heart rate > 100 beats per minute
1.5
Immobilisation for more than 3 days or surgery in the previous 4 weeks
1.5
Previous DVT/PE
1.5
Haemoptysis
1
Malignancy (on treatment, treated in the last 6 months, or palliative)
1
Clinical probability simplified scores
- PE likely - more than 4 points
- PE unlikely - 4 points or less
If a PE is 'likely' (more than 4 points)
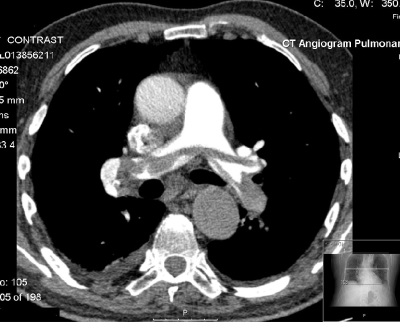
- arrange an immediate computed tomography pulmonary angiogram (CTPA)
-
If there is a delay in getting the CTPA then interim therapeutic anticoagulation should be given until the scan is performed.
- interim therapeutic anticoagulation used to mean giving low-molecular-weight heparin
- NICE updated their guidance in 2020. They now recommend using an anticoagulant that can be continued if the result is positive.
- this means normally a direct oral anticoagulant (DOAC) such as apixaban or rivaroxaban
-
if the CTPA is positive then a PE is diagnosed
- if the CTPA is negative then consider a proximal leg vein ultrasound scan if DVT is suspected
If a PE is 'unlikely' (4 points or less)
- arranged a D-dimer test
- if positive arrange an immediate computed tomography pulmonary angiogram (CTPA). If there is a delay in getting the CTPA then give interim therapeutic anticoagulation until the scan is performed
- if negative then PE is unlikely - stop anticoagulation and consider an alternative diagnosis
CTPA or V/Q scan?
The consensus view from the British Thoracic Society and NICE guidelines is as follows:
- CTPA is now the recommended initial lung-imaging modality for non-massive PE. Advantages compared to V/Q scans include speed, easier to perform out-of-hours, a reduced need for further imaging and the possibility of providing an alternative diagnosis if PE is excluded
- if the CTPA is negative then patients do not need further investigations or treatment for PE
- V/Q scanning may be used initially if appropriate facilities exist, the chest x-ray is normal, and there is no significant symptomatic concurrent cardiopulmonary disease. V/Q scanning is also the investigation of choice if there is renal impairment (doesn't require the use of contrast unlike CTPA)
Some other points
D-dimers
- sensitivity = 95-98%, but poor specificity
- age-adjusted D-dimer levels should be considered for patients > 50 years
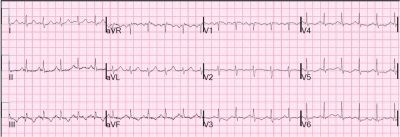
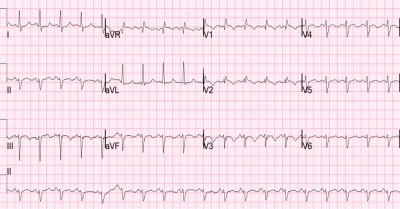
ECG
- the classic ECG changes seen in PE are a large S wave in lead I, a large Q wave in lead III and an inverted T wave in lead III - 'S1Q3T3'. However, this change is seen in no more than 20% of patients
- right bundle branch block and right axis deviation are also associated with PE
- sinus tachycardia may also be seen
Chest x-ray
- a chest x-ray is recommended for all patients to exclude other pathology
- however, it is typically normal in PE
- possible findings include a wedge-shaped opacification
V/Q scan
- sensitivity of around 75% and specificity of 97%
- other causes of mismatch in V/Q include old pulmonary embolisms, AV malformations, vasculitis, previous radiotherapy
- COPD gives matched defects
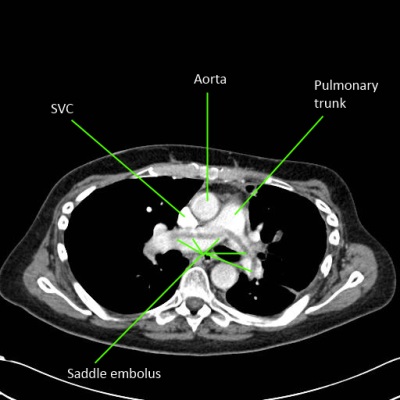
CTPA
- peripheral emboli affecting subsegmental arteries may be missed
- Clinical Characteristics of Patients with Acute Pulmonary Embolism(Data from PIOPED II) Am J Med. Oct 2007; 120(10): 871879.